What tests are required for colorectal polyps?
The doctor may use four tests to check if polyps are present:
- Finger Rectal examination. The doctor, wearing gloves, palpates the rectum, the last part of the colon, to tell by touch if it is normal. This test detects polyps only in the rectum. So the doctor may need to do one of the other tests listed below to detect polyps in the upper parts of the bowel.
- Barium hypo enema. The doctor diffuses a liquid called barium into the rectum before taking x-rays of the colon. The barium makes the bowel look white in the images. Polyps are dark, so they are easy to see.
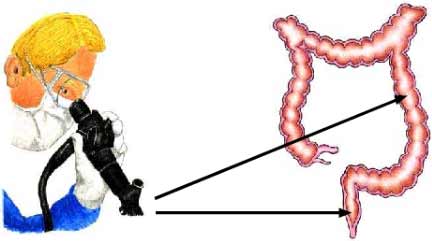
- Sigmoidoscopy. With this test, the doctor looks inside the colon by placing a thin and flexible tube in the anus. The device is called a sigmoidoscope and carries a light and a tiny video camera. The doctor uses the sigmoidoscope to look at the last third of the colon.
- Colonoscopy. This test is similar to the sigmoidoscopy, except that it allows the doctor to look at the entire colon. The examinee is usually given relaxants before the test.
What is Colonoscopy?
Colonoscopy allows the doctor to look inside the entire colon, from the lowest part, the rectum, to the lowest part of the small intestine. This test is used to diagnose unexplained changes in bowel behavior and to detect early signs of cancer in the colon and rectum. It enables the doctor to see inflamed tissue, abnormal growth, ulcers, bleeding and muscle spasms.
To perform the procedure, the examinee lies down on the examination bed on his or her left side, having taken painkillers and mild relaxants in order to be relaxed. The doctor inserts a long, flexible, lighted tube into the rectum and slowly guides it into the colon. The tube is called a colonoscope. The endoscope transmits an image of the inside of the colon so the doctor can carefully examine the lining of the bowel. Also, the endoscope bends so the doctor can move it around the curves of the bowel. The patient may need to change position so that the doctor can move the endoscope where needed. The endoscope blows air into the colon, causing the colon to inflate so the doctor can get a better view.
If there is something abnormal in the colon, such as a polyp or irritated tissue, the doctor may remove part of it using tiny instruments passed through the endoscope. The tissue-biopsy is then sent to the laboratory for examination. If there is bleeding in the colon, the doctor may pass a laser, heated catheter or electrical catheter, or inject special medicines (adrenaline solution) through the endoscope to stop the bleeding.
Bleeding and injury – puncture of the colon – are possible complications of colonoscopy, but they are rare.
The colonoscopy takes between 30 and 60 minutes. The patient is given sedatives and painkillers so that he or she does not suffer. However, he or she will need to stay in the office for 1 to 2 hours until the painkillers wear off.
What are the indications for colonoscopy?
According to the STOP Foundation in Anorectal Cancer:
- From age 45 (it used to be from age 50) onwards, everyone should start having a Colonoscopy and repeat it every 10 years. The test should be done whether someone is completely asymptomatic, i.e. has no symptoms, or has a history of anorectal disease.
- A patient should have a colonoscopy from the age of 40 or earlier if there is a personal or family history or benign anorectal polyps, anorectal cancer, ovarian cancer, uterine cancer, breast cancer, ulcerative colitis or Crohn’s disease.
What is Sigmoidoscopy?
A flexible sigmoidoscopy is a test like a colonoscopy, only it is shorter, as it is limited to the lower one-third of the colon. A sigmoidoscopy allows the doctor to examine the sigmoid colon. The doctor can use this procedure to identify the cause of diarrhea, abdominal pain or constipation. Sigmoidoscopy is also used to look for early signs of cancer in the colon and rectum. With Sigmoidoscopy, the doctor can see bleeding, inflammation, abnormal growth and ulcers.
The sigmoidoscopy takes between 10 and 20 minutes. During this procedure, the examinee may feel pressure and slight cramping in the lower abdomen. However, once the air is expelled from the colon, he or she will feel better.
The discovery of a polyp with the flexible sigmoidoscopy, necessitates the examination of the entire colon with a colonoscope, as at least 30% of these patients will have other polyps.