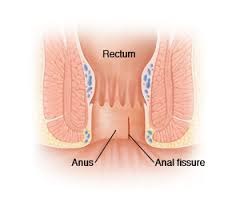
How is anal fissure treated?
At least 50% of anal fissures heal on their own, without the need for surgery. However, the longer an anal fissure remains, the less likely it will be to heal on its own.
Many times, acute anal fissures heal on their own naturally, with good anal hygiene. This means a good cleaning after each bowel movement or filling the area with plenty of lukewarm water.
The use of sitz baths (soaking the anus in plain warm water for 20 minutes, several times a day) helps relieve the symptoms of an anal fissure, but cannot really help the healing process. Applying hydrocortisone topically to the folds of the anus several times a day helps relieve symptoms but slows down the healing process.
A high fiber, well-balanced diet as well as regular defecations offer significant help in the treatment of anal fissure.
Attempts have been made to treat with chemical sphincterotomy, using a wide range of agents including nitric oxide and botulinum toxin. The goal of the treatment is to reduce ischemia by reducing pressure on the rest of the anus and improving blood supply to the mucosa. It is taken for granted that the fissure is characterized by spasm of the internal sphincter of the anus and reduction of mucosal blood flow.
It has been shown that topical application of nitrates reduces pressure on the anal sphincter and improves blood flow to the anal skin. This dual action results in the treatment of anal fissures in more than 50% of patients. The main side effect is headache in 20%-100% of cases.
It has also been shown that local injection of botulinum toxin near the anal sphincter causes denervation, muscle weakness of the sphincter and a decrease in pressure on the rest of the anal sphincter. Which allows the anal fissure to heal. Healing of the anal fussure occurs in more than 60% of patients. The main side effect is, on the one hand, gas and/or fecal incontinence, which lasts up to two months in 2% to 21% of cases, and on the other hand, the possibility of needing a second and third infusion.
What about the surgical treatment of anal fissures
When surgical excision is required, the chronic anal stretch marks are removed along with the papilloma, and adjacent crypts from the underlying muscle. Also, the internal and external hemorrhoids associated with the anal fissure are removed. Usually, the scar tissue in the posterior quadrant of the anus is completely uncovered.
The criteria for excision of anal fissures are: a) long duration and b) association with other rectal diseases such as hemorrhoids, mucosal prolapse, Proctitis/Ulcerations/Inflammatory Bowel Disease, Cryptitis, Abscesses, Fistula, Hypertrophied Papillae, anal tags, polyps, Stricture/Stenosis etc
Sometimes anal dilation is performed to smoothly interrupt the continuity of scar tissue at the base of the anal fissure. Other times cauterization with laser, electrosurgery or a chemical such as silver nitrate is used to expose or resurface the base of the anal fissure. In this way, we encourage new tissue growth and healing of the anal fissure.
Other surgeons use partial internal – lateral sphincterotomy. This surgery consists of a small operation to cut a part of the anal muscle. This helps the anal fissure heal by preventing pain and spasm, which is directly related to healing. By cutting this muscle, we rarely interfere with the ability to control bowel movements.
The choice of surgical technique to treat anal fissures depends on the experience of the colorectal surgeon.
The technique that we choose as the most appropriate for the treatment of anal fissures is laser electrocoagulation of the fissure and its margins, leaving the internal sphincter virtually intact. By these means, we destroy scarred tissue and give the tissue a chance to heal gradually from the bottom to the top of the anal ulcer of the fissure. The patients recover uneventfully and are discharged on the same day.
In Proctoclinic, we have used this laser technique to treat more than 200 patients with anal fissure. All patients experienced immediate improvement and achieved healing of their fissure within one month. We had no case of recurrence of the fissure and all patients remained in excellent condition at their subsequent visits. No complications and no cases of incontinence were observed.