Anal fistula – The most effective treatment
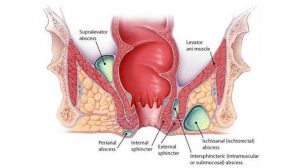
Anal fistula is a sequela of the abscess ulceration or incision drainage that occurs around the anus and rectum, which is manifested as the formation of abnormal channels connecting the anal canal and rectum with the skin around the anus.
Can an abscess cause a fistula?
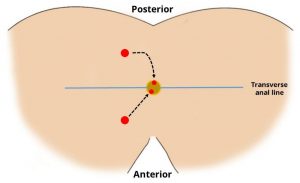
An anal abscess is an infected cavity filled with pus found near the anus or rectum. 90% of abscesses are the result of an acute infection in the internal glands of the anus. Occasionally, bacteria, fecal material or foreign matter can clog an anal gland and tunnel into the tissue around the anus or rectum, where it may then collect in a cavity called an abscess.
An anal fistula (also called fistula-in-ano) is frequently the result of a previous or current anal abscess. This occurs in up to 40% of patients with abscesses. A fistula is an epithelialized tunnel that connects a clogged gland inside the anal canal to the outside skin.
Anal Fistula and symptoms
Anorectal pain, swelling, perianal cellulitis (redness of the skin) and fever are the most common symptoms of an abscess. Occasionally, rectal bleeding or urinary symptoms, such as trouble initiating a urinary stream or painful urination, may be present.
Patients with fistulas commonly have a history of a previously drained anal abscess. Anorectal pain, drainage from the perianal skin, irritation of the perianal skin, and sometimes rectal bleeding, can be presenting symptoms of a fistula-in-ano.
More specifically, the characteristics of an anal fistula are:
- Bloody drainage
- Foul-smelling pus exhibiting along with fever
- No protruding piles
- Constant pain around the anus even without bowel movements
- Recurrent rates are considerably low
- Most cases require treatment interventions
Treatments Of An Anal Fistula
To prevent incontinence or other unpleasant complications, new techniques have been developed to preserve the sphincter and prevent recurrences. The most representative of these are:
- Anal abscess drainage: Under most circumstances, anal abscess can be surgically drained to remove a pocket of pus that has built up within the anal area. However, the rates of anal fistula after the drainage are considerably high, up to 50%
- Sphincter sparing procedures like treatment with fibrin glue
- Anal fistula plug insertion
- Fistula-tract laser closure (FiLaC) is a sphincter-saving technique using a radial emitting laser fiber to obliterate the fistula
- Anal fistula surgeries. Surgical approaches to treat anal fistulas are:
- Ligation of Intersphincteric Fistula Tract or LIFT procedure. The LIFT procedure is a relatively new technique involving ligation and division of the fistula tract in the intersphincteric space, and, usually, brings back quality of life to the patients as continence can be well preserved.
- Fistulotomy
- Seton placement
- Fistulectomy
Which technique of all is superior?
Ligation of Intersphincteric Fistula Tract or LIFT procedure appears to be safe and effective with relatively little injury to the area. Anal fistula plug insertion and fibrin glue, on the other hand, have limited use and low healing rates.
The use of a novel diode laser source and a radial emitting laser probe in addition to conventional surgery is a very promising new technique in sphincter-preserving anal fistula repair. The observed healing rate is high. Due to minimized trauma to the sphincter muscle, there are good short-term functional results without observable procedure-related complications.
Anal Fistula Treatment with Fistula-tract laser closure (FiLaC)
FiLaC® is a novel technique that was developed using a newly invented radial emitting laser probe to destroy the fistula epithelium and to simultaneously obliterate the remaining fistula track.
The main aim of FiLaC® (Fistula – track – LaserClosure) laser treatment is to close the perianal fistula without causing injuries to the sphincter and preserve any part of the sphincter muscle tissue intact, while minimizing the possibility of incontinence.
During the FiLaC® procedure, a small thin laser probe is used to destroy the fistula tissue but does not damage any nearby tissue. This laser probe is very flexible and it is threaded into the fistula tract and then withdrawn as laser energy is being emitted. While the FiLaC® laser probe is being pulled back slowly the tract is being closed. This eliminates the need for a surgeon to try to tediously extract the unwanted fistula tissue during a long complex surgery.
Proctoclinic: A pioneer in the development of FiLaC® technique
Through years of scientific research and perseverance, Proctoclinic has developed and established the use of medical lasers for bowel and rectal treatments. More specifically, we started applying laser therapy in 2012 – first in Greece and among the first in Europe – to almost all our patients. In recent years, after our own modification-evolution of the FiLaC® technique, the healing rate reached a 95%.
The Minimally invasive/nearly painless application and the impressive results gave us the possibility to use the FiLaC® laser probe in other fistulas – medium or low – because the healing time and the patient’s post-operative discomfort is much shorter compared to other techniques.
FiLaC treatment has the following important advantages:
- It ensures good control of the intervention, without trauma, while keeping intact the sphincteric mechanism
- It is applicable to all fistula lengths preserving the functional integrity of the fistula
- The flexibility of the fiber ensures access to fistulas with difficult anatomy
- The operation lasts only a few minutes
- The treatment can be combined with other techniques to close the orifice
- It is the safest treatment with the highest healing rates
- It is applied with absolute safety in patients with Crohn’s disease and multiple fistulas
- Quicker recovery and resuming normal routine