Anal Fissure – Symptoms – Treatment
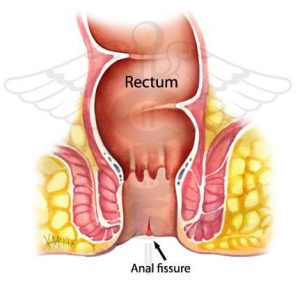
A tear in the skin of the anal wall is known as an anal fissure.Read more
What causes an anal fissure?
Extreme constipation or diarrhea, usually combined with nervous tension over a prolonged period of time, can cause abrasions in the anus, i.e. simple tears such as stretch marks, or acute ulcers on the anal rim. Anal fissures, however, can also be secondary symptoms of bowel diseases such as Crohn’s disease, ulcerative colitis or from an orthopedic surgery, proctitis, tuberculosis, anal cancer, etc. Read more
What are the symptoms of anal fissures?
Usually this injury (tear) of the anus causes severe pain (burning sensation) during defecation and is often accompanied by bleeding and itching. Especially the pain that is triggered during defecation usually lasts for several hours afterwards. In a chronic anal fissure condition the pain may occur up to one hour after defecation. The intensity and duration of the pain does not depend on the size of the tear in the lining of the anus or anal canal.
Patches: The persistence of anal fissures and inflammation over a long period of time (chronic anal fissure) results in swollen skin papillomas developing at both ends of the tear that are usually visible to the naked eye on the anal labia, also known as anal papillomas. (see album)
How is it diagnosed?
Diagnosing anal fissure is fairly easy. A careful overview of the area will often reveal an anal papilloma. After mild separation of the skin of the anal verge, the ulcer may be seen. Often the fibers of the muscle of the internal anal sphincter can be seen at the base of this perforated ulcer.
What conditions is it commonly confused with?
Quite often, spasm of the anal sphincter muscles, known as Proctalgia, can be misdiagnosed as anal fissures. Proctalgia often mimics the appearance of an anal fissure. The difference is that there is no trauma in proctalgia. An anal fissure must also be distinguished from an ulcer caused by Crohn’s disease, leukemia or malignant tumors. Anal fissures are rarely multiple.
How is anal fissure treated?
At least 50% of anal fissures heal on their own, without the need for any treatment. Recently developed anal fissures (acute) are most easily treated – often without treatment, by simply regulating bowel movements and softening stools (through fiber and/or preparations), and by good hygiene of the area (washing with warm or lukewarm water).
Long-standing anal fissures (chronic) are more demanding to treat, as they may persist even after taking medication. In this case, various methods of intervention in the area are followed, such as injection of botulinum toxin (Botox), the use of a modern healing laser or the classic operation of resection of a part of the internal sphincter (lateral internal sphincterotomy).
Read more
Which technique do we use at Proctoclinic?
LASER TREATMENT
In Proctoclinics, we treat anal fissures with laser electrocoagulation of the fissure and its margins, leaving the internal sphincter virtually intact. By these means, we destroy scarred tissue and give the tissue a chance to heal gradually from the bottom to the top of the anal ulcer of the fissure. The patients recover uneventfully and are discharged on the same day.
LASER treatment for anal fissures is the result of specialization, research and many years of experience in a multitude of cases. It is a minimally invasive technique, painless, short lasting and offers great results.
But in addition to this, laser treatment ensures another main advantage: it leaves the anal sphincter intact, thus preventing any complications. Therefore, the application for the treatment of anal fissures is also the safest option – with a short treatment of 10-15 minutes, we achieve a great result and we avoid possible failures caused by Botulinum toxin or more serious complications such as sphincterotomy